- Oct 17, 2025
When Sex Hurts: Understanding Painful Penetration, Pelvic Tension, and the Path to Healing
- Brittney Ellers
- Pelvic Health + Healing
- 0 comments
As a holistic pelvic floor physical therapist, I’ve met so many women who have quietly carried this pain. They think it’s “just how my body is,” or they’ve been told to just relax or have a glass of wine (which, let’s be honest, helps no one).
What most people don’t realize is that pelvic pain during or after sex isn’t “normal.” It’s actually a sign that your body is communicating — often trying to protect you. (Curious about other ways your body may be talking? Check out my free checklist here.)
The best part? It’s absolutely treatable.
Pelvic Floor Pain During or After Sex
There are many kinds and causes of pelvic pain, but the two that show up most often in my practice are called vaginismus and dyspareunia. These terms might sound clinical or intimidating, but naming what’s happening in your body can be deeply empowering. It gives you language for something you may have been feeling for years. It can also feel like a ton of bricks that's landed in your lap. But let's again reiterate — these diagnoses do not have to become life-long sentences, we can work through this! But let's break them down a little first.
What Is Vaginismus?
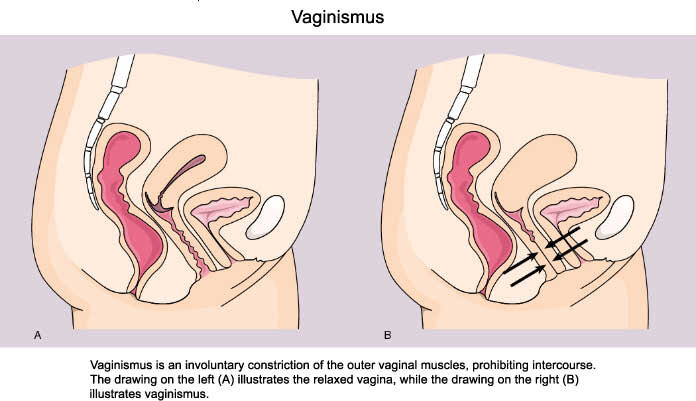
Vaginismus is defined as the involuntary tightening of the vaginal muscles that makes penetration painful or even impossible — whether that’s during sex, using a tampon, or having a pelvic exam (1).
I remember the first time I met someone with vaginismus. It was during my first pelvic floor continuing education course, and my lab partner — who bravely volunteered for an internal assessment — shared that she had only recently been able to use tampons in her mid-twenties. That moment opened my eyes to how many people experience this pain quietly, often without knowing it has a name.
Those with vaginismus often want intimacy, but their bodies say “no” before their minds can. It’s not about lack of desire — it’s a protective reflex, rooted in fear, anxiety, or past experiences that live in the tissues. For some, this pattern is primary, meaning they’ve never been able to tolerate penetration. For others, it’s secondary — they once could, but now their body reflexively tightens or “pushes out” in anticipation.
I’ve also seen how cultural and religious conditioning can shape this reflex. This was part of my own story — growing up in a faith-based household where sex before marriage was framed as taboo or shameful. When pleasure and intimacy are met with fear or silence, the body can internalize that message and hold it in the pelvic muscles.
As one study notes, women who haven’t been able to consummate their marriages due to primary vaginismus may have “excessive closeness of family members, allowing the family to be intrusive and exercising pressure on the couple, a strict education which highly values virginity, transmits fear of ‘the male’ and fear of sex, linking sex with pain” (2).
This resonates deeply with conversations I’ve had with friends who were also raised in conservative or religious environments. So many of us are still unlearning those early imprints — learning to meet our bodies with curiosity, gentleness, and permission instead of fear. It’s one of my favorite topics to unpack, and I look forward to continuing to explore it in upcoming workshops and conversations.
What Is Dyspareunia?
Dyspareunia is pain that happens with sexual activity — at the entrance, deeper inside, or even after intercourse. It might feel like a burning, stinging, or sharp-as-glass sensation. Not ideal, to say the least.
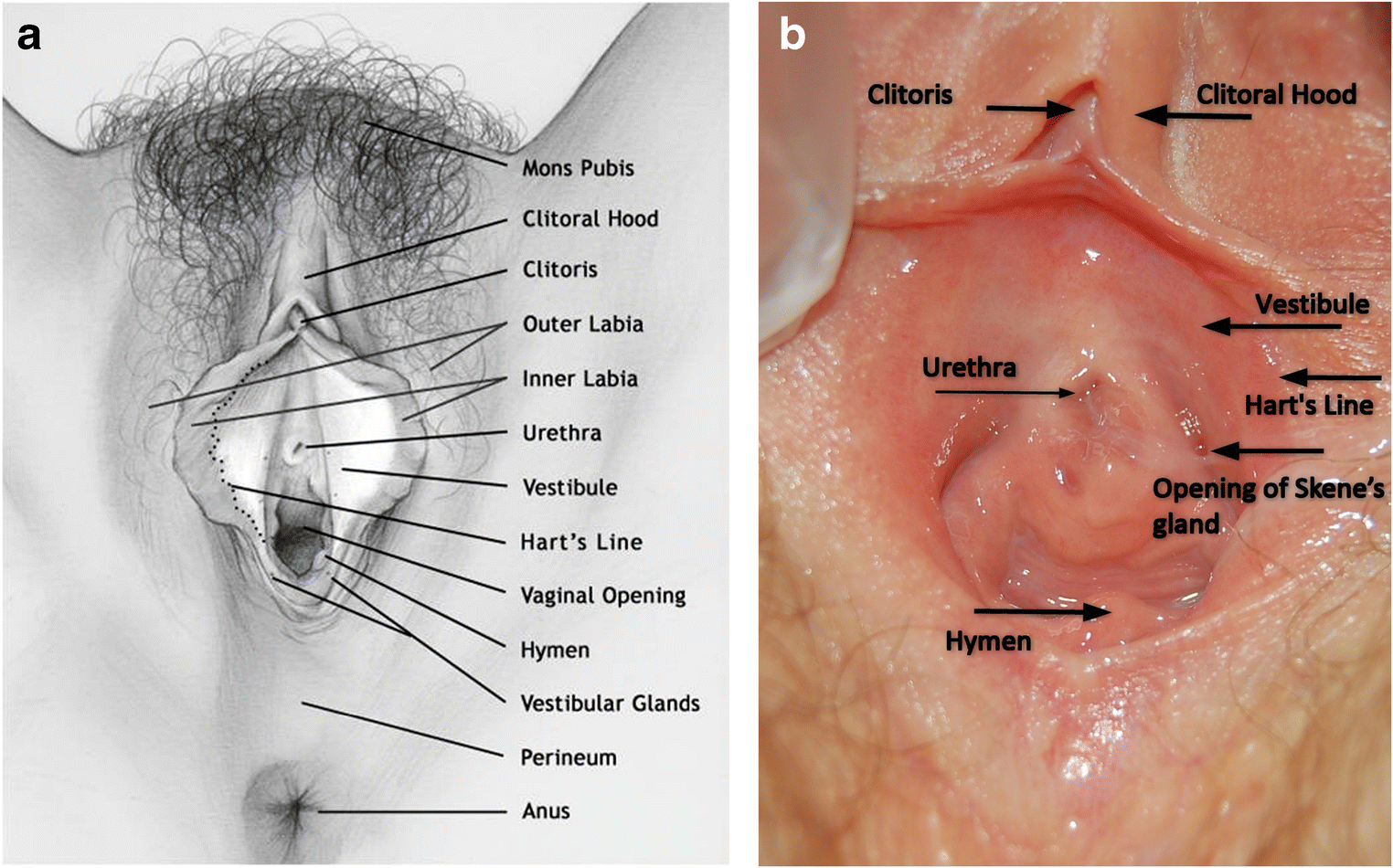
One of the most common types is called provoked vestibulodynia, where even light touch at the vaginal opening with a Q-tip can feel unbearable (look for the areas in the images below for "vestibule" on the inside of the inner labia). Sometimes, the pain is caused by overly tight muscles; other times, by scar tissue, hormonal changes that thins out the tissue, or inflammation.
Here’s the tricky part: vaginismus and dyspareunia often overlap. In fact, research shows they can be nearly impossible to fully separate (3). The Journal of Psychosomatics Obstetrics and Gynecology suggests a multi-axial description of these syndromes (a cluster of signs and symptoms grouped together), rather than having them separate. That’s why I prefer to think of them on a non-linear spectrum — the body’s way of communicating that it doesn’t yet feel safe to open.
How Pelvic Floor Dysfunction Develops
Pelvic pain rarely has one single cause. It’s a blend of physical, emotional, and relational factors.
It can stem from:
Trauma, surgeries, or painful experiences (even those we may not consciously remember)
Fear, shame, or anxiety around sex
Hormonal shifts, postpartum changes, or perimenopause
Birth injuries or scar tissue
Stress patterns that keep the body in “fight or flight”
Lack of arousal or rushed penetration
Your pelvic floor is deeply intertwined with your nervous system and your subconscious. When your body senses threat, or what feels like a demand of your energy and body — even subtle emotional stress — your pelvic muscles can tighten to protect you. Healing begins when your body learns that it’s safe to soften again.
Treatment and Support
Pelvic floor physical therapy can be life-changing for those experiencing these conditions. Treatment is gentle, respectful, and deeply individualized. There has to be patience. There is no forcing here. Some of the approaches I use include:
Diaphragmatic breathing and relaxation techniques to calm the nervous system, including craniosacral therapy
Manual therapy and intravaginal release work to help the muscles learn safety again
Dilator or wand work protocols to reintroduce sensation gradually
Somatic and sensate focus exercises to rebuild connection and pleasure
Collaboration with other providers (sex therapy, trauma work, or hormonal support)
Through consistency and compassion, many of my clients experience full relief — and beyond that, a new relationship with their bodies and their pleasure.

Try This Now: Reconnecting with Your Pelvic Floor
If you’re experiencing pain, start with awareness — not fixing. Here are a few practices to begin cultivating safety and softness:
1. Breathe low and slow.
Place your hand on your lower belly and breathe into your pelvis. Imagine the breath expanding your vaginal walls like a flower opening with each inhale. Exhale and imagine everything softening.
2. Practice pelvic presence.
Throughout the day, pause and notice your pelvic floor. Is it gripping? Can you let it go, even 5%?
3. Redefine touch.
If partnered, remove penetration from the equation. Explore touch that’s focused on curiosity and connection — not performance or a goal.
If solo, begin with gentle external exploration using a mirror or your hands, not to “do” anything, but to listen.
Practice listening and reconnecting with your pelvic floor with this free guided meditation.
These exercises are a small preview of what we explore more deeply in my live workshops and courses — including how to safely reawaken sensation, pleasure, and connection to your pussy’s wisdom.
You Are Not Alone
If you’ve been avoiding sex, exams, or even your own touch because of pain — I want you to know this: there is nothing “wrong” with you. It's wildly common: a staggering 75% of women will experience painful penetration at least once in their lives. Your body has been doing what it knows to do to keep you safe. And with the right guidance and care, that same body can relearn how to open, receive, and feel deeply again.
Healing this part of yourself is sacred work — it’s body, mind, and spirit work.
Ready to Go Deeper?
If this resonates, here are two beautiful next steps:
🐱 Why a Tight Pussy Ain’t It (And How to Fix It)
A workshop for the woman who’s been holding — emotionally, physically, and energetically — and wants to understand how tension shows up in her pelvic floor. You’ll learn how “tight” doesn’t mean “toned,” and how to restore fluidity and flow to your body and pleasure.
🌹 Numb to Nourished: Why You Might Need to Break Up with Your Vibrator
If you’ve been feeling disconnected, shut down, or numb in your sensuality (with a vibrator or not), this workshop experience guides you through the journey of softening back into sensation. It’s about rebuilding trust with your body and rediscovering pleasure as your birthright.
You deserve to feel safe in your body.
You deserve pleasure that feels fulfilling. Nourishing. Life-giving.
Don't give up. I promise, it's worth it.
xx
Dr. Brittney

Resources
Crowley, T, Goldmeier, D, Wadsworth, J, Hiller, J. Clinical Review: Diagnosing and Managing Vaginismus. BMJ 2009;338:b2284.
Zgueb, Y., Ouali, U., Achour, R., Jomli, R., & Nacef, F. (2019). Cultural aspects of vaginismus therapy: A case series of Arab-Muslim patients. The Cognitive Behaviour Therapist, 12, E3. doi:10.1017/S1754470X18000119
-
Marie-Andrée Lahaie SCB. Vaginismus: A Review of the Literature on the Classification/Diagnosis, Etiology and Treatment - Marie-Andrée Lahaie, Stéphanie C Boyer, Rhonda Amsel, Samir Khalifé, Yitzchak M Binik, 2010. SAGE Journals. https://journals.sagepub.com/doi/full/10.2217/whe.10.46. Accessed January 17, 2021.